After the government pledged to spend more on mental health, those in smaller towns say they’ve yet to see it

Image Provided
INVERNESS, U.K.—Peter Todd lives in the far northern county of Caithness in the Scottish Highlands and is an outspoken survivor.
He was one of the young children victimized in a widely publicized pedophile scandal involving British member of parliament Cyril Smith. Smith died in 2010, before investigations concluded on the 29 people who’d come forward with allegations of abuse against him. Todd says it’s been a long battle to recover and that he’s struggled with depression his whole life.
But his attempts to receive treatment, he says, have been met with repeated disrespect from the Scottish government.
Coming from the town of Thurso, Todd has to make a 220-mile, five-hour round trip to New Craig’s Psychiatric Hospital in Inverness. He used to stay at a patient accommodation next to the facility. But when he arrived in the summer of 2018, he was told he could not stay there, despite having a reservation, due to supposed antisocial behavior. He was later cleared of any wrongdoing by the legal organization Ombudsman and issued a letter of apology by National Health Service – Highland, but still is not allowed to stay in the facility.
Instead, he is forced to pay for hotels and Airbnbs out of his pocket and then request reimbursement by the government’s healthcare system. According to Todd, not allowing him in patient accommodations has cost the Scottish government £40,000.
Todd said he sees his experience as just one example of how the nationalized healthcare system fails those needing mental health care.
“Mental health services are the Cinderella service of the NHS. It’s underfunded, it’s badly managed and it’s centralized. And it’s not patient-centered.” Peter Todd, Scottish patient from Thurso
“Mental health services are the Cinderella service of the NHS. It’s underfunded, it’s badly managed and it’s centralized. And it’s not patient-centered,” he says. “Because they centralize stuff, that means there’s a barrier to access treatment. The amount of time I’ve had to spend in Inverness is extraordinary because of the centralization model.”
Experts and many patients agree, Scotland’s mental health system is in crisis. Scotland reports the highest rates of suicide in the U.K. and rural areas are often double the rate of places like London. Citizens in the sparsely populated Highlands and islands of Scotland have complained that the NHS centralized healthcare in the cities, increasing waits in rural areas for care, including crisis therapy.
In January of this year, the Royal College of Psychiatrists in Scotland produced a report that requested increased funding for mental health services in the 2025-26 Scottish budget.
“Mental health services in Scotland are under unprecedented pressure, with demand vastly surpassing resourcing,” the report said. It further reported that the 2022 Scottish Census found the number of people reporting a mental health condition in Scotland “has more than doubled since 2011,” rising from 4.4% to 11.3% of the 2022 population.
The ruling Scottish National Party pledged to commit 10% of health funding to mental health during the parliamentary campaigns in 2021.
Instead, the Royal College of Psychiatrists reports the percentage of investment continues to fall, from 9.12% in 2011 to 8.53% in 2022. That is £238.5 million short of 10%.
These budget shortfalls come at a time when Scotland has the highest suicide rates in the U.K. with 14 deaths per 100,000 people. Wales is second with 12.5 deaths and England is the lowest with 10.5.
The 2023 probable suicide statistics show there were 2.5 times more deaths by suicide in the most rural areas of Scotland than in the least rural areas.
In the last six years, the highest rates of suicide by NHS board area have been in the Orkneys, Highlands, Tayside and Western Isles, some of the most remote places in Scotland. The Royal College of Psychiatrists’ report also notes that these areas also had some of the lowest investment in mental health services by the regional organizations choosing how to allocate their health dollars, with Orkney only committing 2.53% of its budget.
Those on the ground express frustration with the overall state of healthcare in these areas.

Image provided
“Remoteness from the center should not mean you get less quality healthcare,” says Iain Gregory, the vice-chairman of the Caithness Health Action Team, or CHAT, a community advocacy group. “Up to 20 years ago, we had local hospitals everywhere. Now we don’t, it’s all been centralized. It’s a political decision.”
CHAT is a group of volunteers, some who have health experience and some who don’t, who campaign for an equitable, accessible and affordable healthcare system. Gregory, who joined CHAT in 2024, feels that mental health care in Caithness is lacking and that Covid emphasized the need for people to be able to access mental health care easily.
He says people who require counseling have a very long wait and care is often given by video link, which he doesn’t feel is adequate for people suffering from mental health conditions.
Gregory echoes Todd’s concerns about the Scottish government minimizing mental healthcare for too long. He says they’ve been allowed to do that “because it is not so obvious,” he says. “Unlike a broken leg, it gets overlooked.”
As an example, he talks about how long it took to replace the local psychiatrist in Caithness, who covers a wide area.
“We have quite a high number of young people who have taken their lives over the last few years,” he says. “We believe that in a county of over 20,000 people, over 20 young people have taken their lives in the last few years.”
Based on CHAT’s data, that would put Gregory’s area at nearly five times the suicide rate in Scotland’s rural counties and nearly 10 times the rate experienced in England.
“We need to bring attention to mental health care the same as emergency care. If someone is in crisis, they need help, and they need that help right now. The only emergency care available right now is the police,” Gregory says. “The effects on people in remote areas are pretty serious.”
The situation that Gregory sees in the far northern tip of Scotland is echoed by advocates on the Western Isles, made up of the isle of Barra, North and South Uists, Benbecula and Harris and Lewis.
“More money is spent closer to the main population center,” city councilor Kenneth Maclean on the Isle of Barra says. “Less is spent the further away you are. I can probably get to New York and back in the time it takes to get to Stornoway (the main town in the Outer Hebrides), for minor things like a 10-minute scan. If the weather kicks in, you can be up there four or five days.”
Though people living in rural areas have to accept that that lifestyle is not always going to be easy, Maclean said, “I think there should be more help. There used to be more help, we used to have far more services here. It’s not that we’re asking for more, we’re just asking for what we had.”
But the centralization of services has caused the Western Isles to lose many of theirs.
Maclean says there is a hospital on the island that Health Secretary Nichola Sturgeon visited 17 years ago and promised to replace. Barra, a town of 1,300 people, asked for upgrades but haven’t gotten any.
The lack of progress in improving care in Barra prompted the Labour member of the Scottish parliament to lament two years ago in a local news site in the Western isles, “There is absolutely no back-up plan or sense of urgency about meeting Barra’s needs.”
Gone, too, is a community psychiatric nurse, or CPN. Now they only come on the ferry when needed.
“When someone threatens suicide then disappears, there’s no time to wait for the CPN to get here on a ferry,” he says. Approximately half the year, it is too windy for the ferry to come in or even for the coast guard helicopter to fly in.
“The stripping of services, that’s what it all boils down to,” he says.
With scarce resources flowing to mental health in many of these communities, nonprofits and community organizations are trying a patchwork of solutions to try and alleviate the crisis.
One example is the charity Change Mental Health, which has set up training to aid those working in rural communities. In 2017, they set up the National Rural and Islands Mental Health Network, an online seminar held nine times a year to support collaboration between individuals and practices. The network helped the National Farmers Union set up their employee mental health training.
“It’s not just [the government’s responsibility], for suicides its everybody’s business to tackle that,” Jim Hume, the convenor of the rural mental health network, says. “There’s so much work going on we’re hoping to see [suicides] drop off.”
Other groups are also trying to step in with services and resources.
Samaritans is a U.K.- and Ireland-wide suicide hotline with volunteer call-takers. In 2023, the Samaritans had 20,000 volunteer call-takers, with 1,300 volunteering from prison.
In conjunction with the Caithness Health Action Team, the Scottish Association of Young Farmers Clubs, Scotland’s largest rural youth organization, currently has a campaign called, “Are Ewe Okay?” Its website provides emergency and non-emergency mental health support and stories from other rural citizens who have struggled with depression and thoughts of suicide.
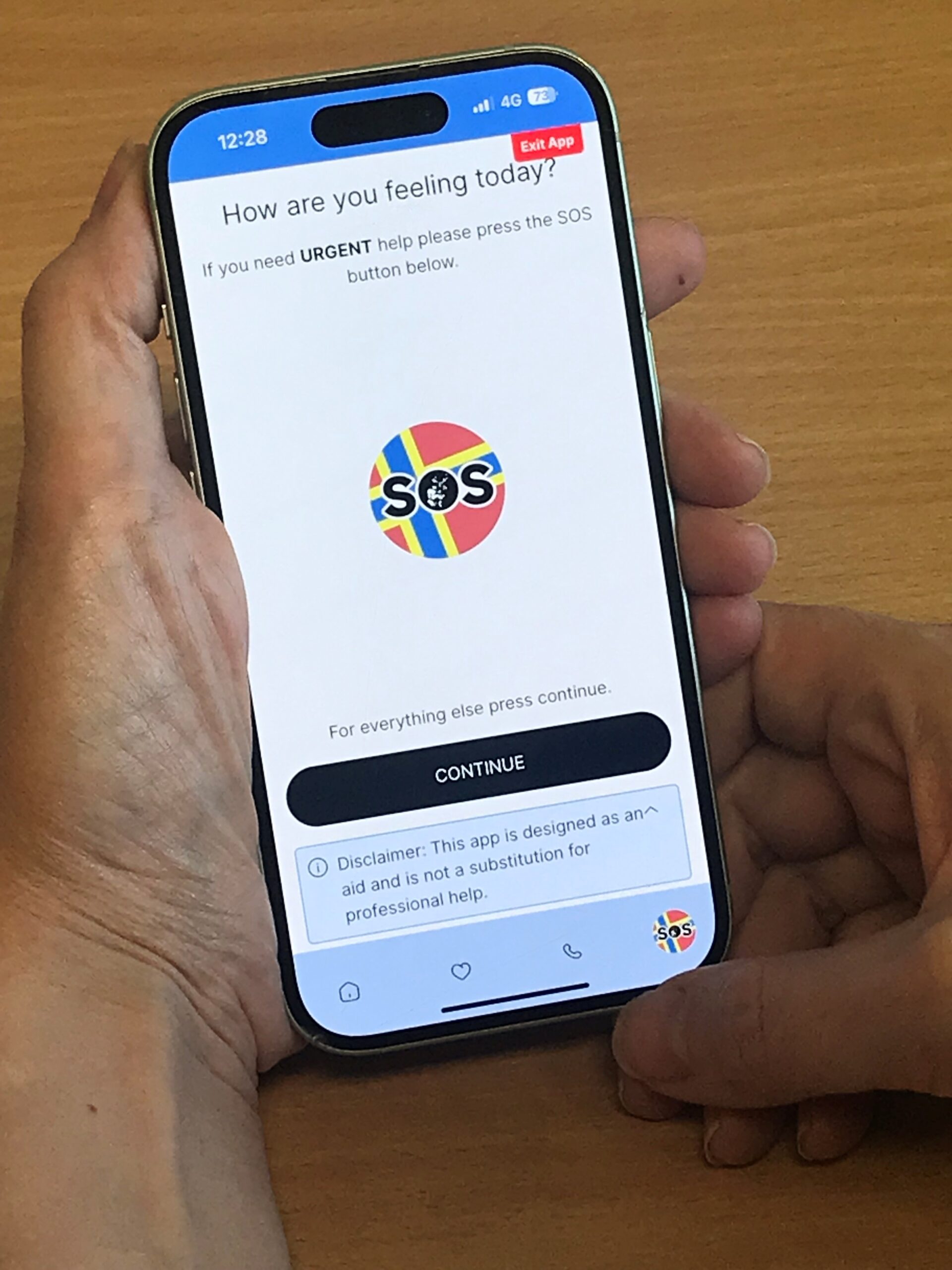
Up in the Orkneys, Callan Curtis works for the local branch of the Health and Social Care Partnership, a coalition of health and social care organizations in Scotland. He provides community care and support services in the Orkney Islands, one of the most rural areas of Scotland and one of the ones most affected by suicide. In March 2025, he helped launch SOS Orkney, a mental health resources and suicide prevention app, as a way for those in crisis to find access to the resources in the rural area that are available.
The Orkneys, which has a population of just under 22,000 spread across 20 inhabited islands, had 42 suicides between 2013 and 2023, many of which were farmers and fisherman; most were people under the age of 27. They built the app to allow people to access resources without having to report their name or go into an office.
“When someone’s neighbor or family member works for the mental health care resources, they don’t want to use it,” Curtis says. “That is why SOS Orkney is anonymous. National services are there to fall back on.”
Since its release in March, the support page listing resources gets 164 views per week.
Currently, Curtis reports that those seeking mental health treatment are told to expect a four-month wait and adds, “The reality is much longer than that.”
Communities like his cannot wait this long, he says, and the various organizations that are not the NHS are trying to do what they can. Suicide in these rural communities hits hard.
“We have such a small community,” Curtis says. “When we lose someone here, we feel it.”
This story is part of a healthcare series produced by the International Reporting program at the University of Montana School of Journalism. Read more from this Scotland-based project, as well as reports from other countries, at Montana Journalism Abroad.